Where global health challenges like pandemics, chronic diseases, and health inequities persist, traditional top-down research models—where experts design studies from afar and impose solutions—are increasingly seen as insufficient. Enter community-driven research, often formalized as Community-Based Participatory Research (CBPR), a collaborative approach that places communities at the heart of the research process. This method equitably involves community members, researchers, and stakeholders from the outset, ensuring that studies address real needs, respect local contexts, and foster sustainable change. Unlike conventional research, which might prioritize scientific rigor over cultural relevance, CBPR emphasizes mutual learning, power-sharing, and action-oriented outcomes.
The transformation brought by community-driven research is profound. It has shifted paradigms in global health by empowering marginalized groups, improving intervention effectiveness, and influencing policy. For instance, during the Ebola outbreaks in sub-Saharan Africa, community engagement strategies that incorporated local leaders and survivor testimonials dramatically enhanced case detection, isolation, and treatment uptake, with combined interventions proving more effective than isolated efforts. Similarly, in the COVID-19 pandemic, rapid evidence reviews from past epidemics highlighted how involving community actors in planning, communication, and surveillance led to context-specific measures that addressed equity for vulnerable populations. This blog explores how CBPR is reshaping global health through its principles, real-world examples, benefits, challenges, and future directions. By drawing on specific case studies from diverse regions, we’ll see how this approach not only generates knowledge but also builds resilient health systems worldwide.
What Is Community-Driven Research?
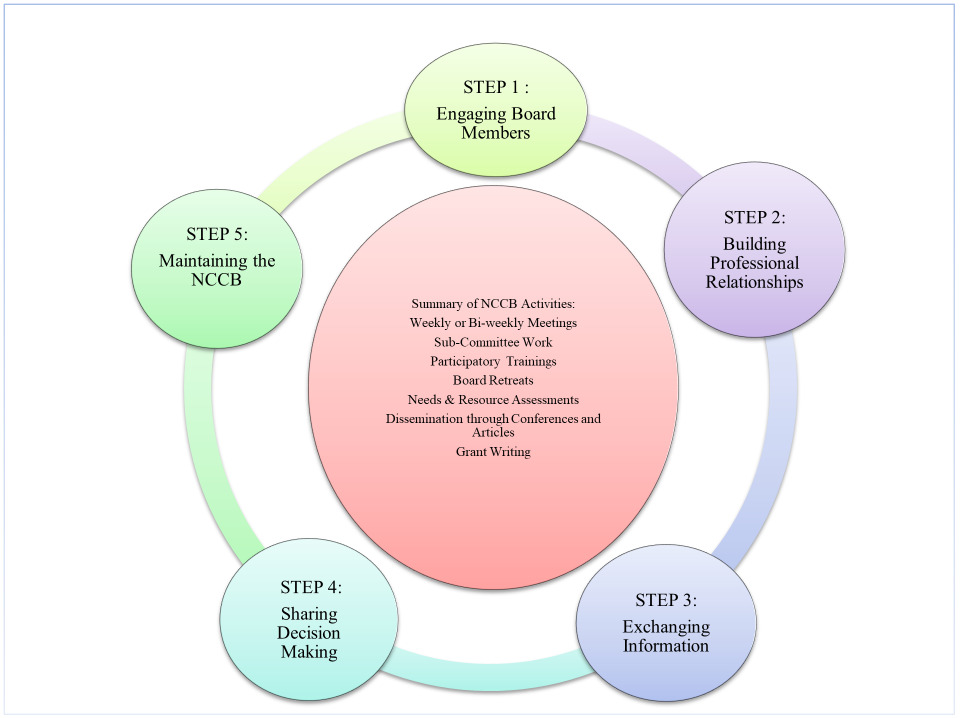
Community-driven research, or CBPR, is a collaborative framework where community members are co-researchers rather than mere subjects. It originated from action research traditions in the mid-20th century but gained traction in public health during the 1990s, influenced by social justice movements and critiques of colonial research practices. CBPR is defined by nine core principles: recognizing community as a unit of identity, building on strengths and resources, facilitating collaborative partnerships, integrating knowledge and action for mutual benefit, promoting co-learning, involving cyclical processes, addressing health from positive and ecological perspectives, disseminating findings to all partners, and committing to long-term sustainability.
In global health, this means research is tailored to local realities. For example, in low- and middle-income countries, CBPR addresses systemic inequities by incorporating indigenous knowledge and cultural practices. Unlike traditional models, where researchers extract data and leave, CBPR fosters ongoing relationships. A scoping review of 26 long-standing CBPR partnerships (lasting over four years) across the U.S. and Canada revealed common focuses on health disparities like cancer, HIV, and diabetes in diverse populations such as African Americans and American Indians. Methods often include partner assessments, interviews, and shared governance, leading to outcomes like policy changes and enhanced community capacity.
This approach is particularly vital in global health because it bridges gaps between evidence and implementation. In developing countries, where resources are scarce, CBPR ensures interventions are feasible and culturally acceptable. For instance, in Thailand, a community-based intervention for hypertension involved health service supports, home visits, and group activities, resulting in improved management strategies. By democratizing research, CBPR transforms passive recipients into active agents of change, ultimately leading to more equitable health outcomes.
Historical Evolution and Key Principles
The roots of community-driven research trace back to Paulo Freire’s participatory action research in the 1970s, which emphasized empowerment through dialogue in Latin America. In global health, it evolved amid criticisms of Western-centric studies that ignored local contexts, such as during the HIV/AIDS crisis in the 1980s. By the 2000s, organizations like the World Health Organization (WHO) advocated for community involvement in health initiatives, recognizing it as essential for achieving the Millennium Development Goals.
Key principles guide CBPR’s evolution. First, equity in partnerships ensures power-sharing, as seen in the development of research ethics codes co-created with communities. Second, cultural humility requires researchers to learn from communities, integrating traditional knowledge. Third, sustainability focuses on long-term impacts beyond funding cycles. A global perspective review on power in participatory health research highlighted how co-production in low-income settings addresses imbalances, with examples from Africa and Asia emphasizing dialogue and shared decision-making.
In practice, these principles have driven transformations. In Indigenous communities, frameworks like Canada’s OCAP® (Ownership, Control, Access, Possession) ensure data sovereignty, shifting from extractive to respectful research. Similarly, in Peru’s Waynanuna Oral Health Project, partnerships with local municipalities and schools incorporated needs assessments and cultural interventions, leading to sustained oral health improvements. This evolution underscores CBPR’s role in decolonizing global health research, making it more inclusive and effective.
Case Studies in Action
To illustrate CBPR’s transformative power, let’s examine specific examples from diverse global contexts.
The Kahnawake Schools Diabetes Prevention Project (Canada)
In the Kanien’kehá:ka (Mohawk) community of Kahnawake, Quebec, the KSDPP began in 1994 amid alarming diabetes rates—12% in adults aged 45–64, double the national average. This CBPR initiative partnered community organizations, schools, hospitals, and academic researchers to promote healthy eating, physical activity, and supportive environments, infused with Indigenous values like collective responsibility and holistic health.
Processes unfolded in four social movement stages: emergence (awareness and partnership formation), coalescence (governance via a Community Advisory Board and ethics code), momentum (expanded interventions, over 100 annually, with national recognition), and maintenance (norm integration despite funding cuts). Methods included document reviews, talking circles with 24 stakeholders, and consensus decision-making. Outcomes were significant: shifted community norms viewing diabetes as preventable, increased collaborations, leadership development (e.g., board elections), and sustained policies like school nutrition guidelines. Challenges like staff turnover were addressed through renewed leadership nurturing, demonstrating CBPR’s adaptability in Indigenous settings.
CBPR in South Africa: Addressing Cervical Health in Cape Town
In an under-resourced Cape Town community, CBPR reshaped research on cervical cancer screening by engaging stakeholders to broaden the focus to “cervical health,” incorporating HIV, STDs, and social determinants. Partners included health professionals, educators, traditional healers, and women’s groups.
Methods involved extensive consultations, informal interviews, and 27 focus groups with 181 participants (youth, mothers, educators). Challenges included language barriers (separate Xhosa and Afrikaans groups) and low attendance due to logistics. Key findings revealed intersecting barriers: poverty driving risk behaviors like sexual bartering, pervasive violence, substance abuse, and apartheid legacies fostering distrust. Strengths included resilient family networks and community groups. Outcomes: a multi-generational intervention framework aligned with national policies, highlighting how CBPR uncovers holistic issues for targeted solutions in developing countries.
Community Engagement in Ebola Outbreaks (Sub-Saharan Africa)
During the 2014–2016 West Africa Ebola epidemic, community engagement was pivotal in Guinea, Liberia, and Sierra Leone. Success hinged on survival rates, survivor testimonials, risk perception, and leader inclusion. Initiatives like the Social Mobilisation Action Consortium used local radio, leaders, and youth for messaging, surveillance, and trust-building.
Combined interventions improved knowledge, attitudes, case detection, and treatment uptake more than singular efforts. For example, health committees handled screening and communication, while community groups supported safe burials. These lessons informed COVID-19 responses, emphasizing early, context-specific involvement.
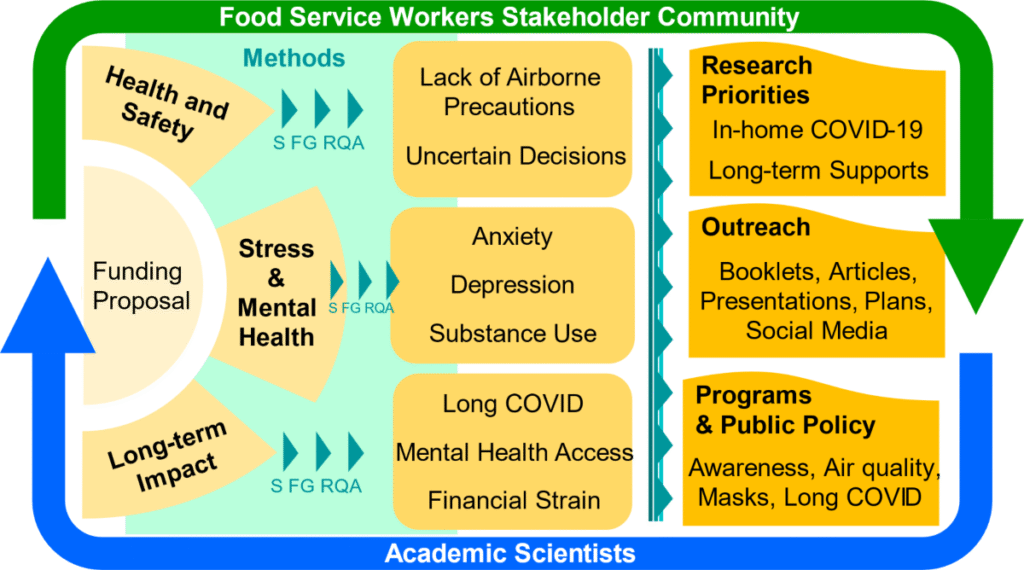
CBPR During COVID-19: A U.S. Community-Academic Partnership
An illustrative COVID-19 CBPR example involved African American churches in the U.S., deploying emergency preparedness within existing partnerships. Actors like faith leaders and health committees facilitated risk communication, surveillance, and logistics.
A rapid review of 37 initiatives from past epidemics (mostly Ebola) showed multifaceted engagement—planning, trust-building, behavior change—led to equitable outcomes for marginalized groups. In Zika responses, resident committees reduced sources via community-led actions. For COVID, digital tools like WhatsApp enabled dialogue under restrictions, underscoring CBPR’s flexibility in pandemics.
These cases show CBPR’s global applicability, from chronic disease prevention to crisis response, yielding culturally resonant, sustainable impacts.
Benefits and Impacts
CBPR’s benefits span individual, organizational, and community levels, driving transformative global health changes. At the personal level, community partners gain skills, confidence, and empowerment; for researchers, it fosters cultural humility and broader perspectives. Organizationally, it builds capacity through shared resources and infrastructure, leading to high recruitment and retention rates in studies. Community-wide, it yields tangible outcomes like policy shifts, reduced disparities, and enhanced trust in health systems.
Impacts are evident in improved health metrics. In the KSDPP, norm shifts reduced diabetes stigma and promoted wellness. In South Africa, uncovering social determinants led to holistic interventions addressing poverty and violence. Globally, CBPR has influenced policies; a conceptual model linking CBPR to policymaking showed how processes like coalition-building result in equitable laws. In pandemics, it boosted surveillance and compliance, as in Ebola’s community-led actions that curbed spread.
Broader impacts include sustainability and equity. Long-standing partnerships create lasting infrastructure, capitalizing on research for ongoing benefits. In vulnerable populations, it amplifies voices, as in Indigenous projects integrating traditional practices for better outcomes. Overall, CBPR transforms global health by making research relevant, actionable, and just.
Challenges and Solutions
Despite its strengths, CBPR faces hurdles. Power imbalances persist, with researchers often holding more credentials and funding control, making equal partnerships elusive. Misunderstandings about goals can strain relationships, while academic demands like control groups clash with community preferences. Sustainability is challenged by funding shortages, staff turnover, and external disruptions like pandemics. In global contexts, cultural and language barriers, as in South Africa, complicate engagement.
Solutions involve building trust through reciprocity and community-led ethics, like OCAP®. Memorandums of understanding can formalize equity, though they must be co-drafted. For sustainability, integrate projects into local systems and nurture champions. In pandemics, adapt with digital tools. Training researchers in humility and providing detailed guidance on challenges can mitigate issues.
The Role of Technology and Future Directions
Technology amplifies CBPR’s reach. Decentralized Science (DeSci) platforms, using blockchain for transparent, community-driven research, are emerging. For example, Bio Protocol enables global collaboration on health issues like microbiome research and kidney disease, tokenizing contributions for equitable benefits. AI agents facilitate data analysis in real-time, as in Spectruth DAO’s PTSD healing initiatives.
Future directions include scaling CBPR for climate-health intersections and integrating it into global agendas like the Sustainable Development Goals. With ongoing student showcases and partnerships, like Duke Global Health Institute’s projects, the field is poised for growth. Embracing hybrid models with tech will enhance accessibility and impact.
Conclusion
Community-driven research is revolutionizing global health by centering voices that matter most. From Kahnawake’s diabetes prevention to Ebola’s community surveillance, CBPR delivers relevant, equitable solutions. While challenges like power dynamics exist, its benefits—empowerment, sustainability, policy influence—far outweigh them. As we face future threats, embracing CBPR with technological innovations will ensure healthier, more resilient world. The key? Listen, collaborate, and act together.



